Pain in my left arm signaled something wrong with this seventy-something body. The doctor ordered tests. “Take some Ativan before you come,” he said, “to lower your blood pressure.” Just four minutes on a treadmill predicted a serious heart attack. He ordered a catheterization. The cardiologist called the day before to reassure me. I would be myself again. My husband had a stent years ago and cleaned the basement drains the next day. I could live with that. I could live.
I chatted briefly with the nurse and entered la-la land. Later, the doctor was not smiling. The heart muscle and other vessels looked pretty good, but the major arteries showed a tight community of plaque like that which killed my father at sixty-two. The pictures said it all: bypass. CABG, they call it, coronary artery bypass graft. Three days before surgery I cleaned the attic, shoveled snow, returned library books, and finished the book I was writing—all to ease my anxiety.
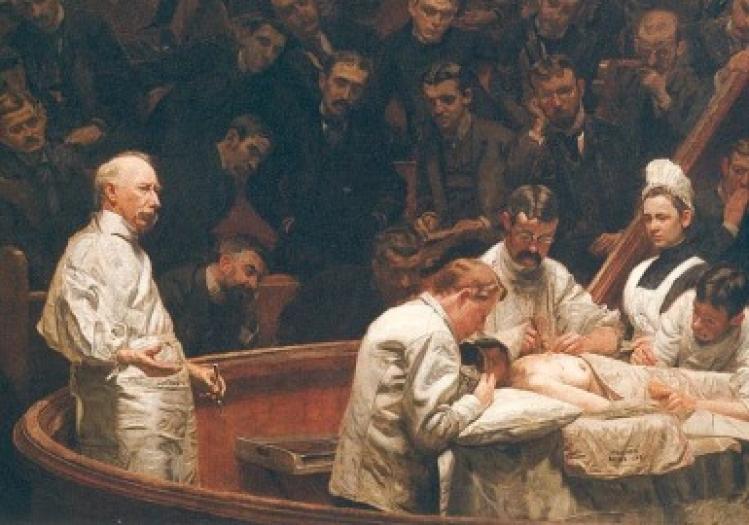
They invaded me with tubes. They stayed the bloody traffic of my heart and rearranged its roadways. They cracked my chest, pumped me with morphine, someone else’s blood, lidocaine and lactose, glucose and glue. Family stood silently by. Finally they removed tubes, leaving tracks of tape and torn skin. They moved my body—was it still my self?—to a step-down room. After two more days they retrieved the remaining wires, took more pictures, and pronounced me “discharged.” No more sleeping on the back of a sheeted rack that hospitals call a “bed.”
But who came home? Was I the same person, or had she died when my heart stopped? The random winter fly in the house was drawn to the cadaverous smell of the surgical site. It seemed to believe I no longer existed.
Appointments with cardiologist and surgeon followed. The old me would have persisted when these men interrupted my questions with their medical wisdom. Now I felt infantilized, muzzled, and frustrated. I felt diminished when others told me when to walk, what to eat, what pills to take and when.
Although only a small scar remains where they took the left radial artery, I wonder if the complete I will live again? Is there a born-again me? There is still a pulse on the right wrist, but the left is silent. The arteries that nourished six children have been diverted to supplant crippled heart vessels clogged to worthlessness. The long scar down my torso reminds me of my expiration. I have been rerouted from my natural course toward death. It feels wrong.
Maybe there is efficacious work ahead. Survival from surgery, survival not only from the physical pain and mutilation but from the pain I see in the eyes of those who love me. My husband has suffered far more than I.
There is also the work of mourning my old life. Before the surgery I was prepared to die. “Please,” I told the surgeon, “if I go sour, let me go. I do not want to live a vegetable life.” We agreed to the lie that no resuscitation would be attempted in the OR. Every ethicist knows that even clear advance directives are suspended in the surgical suite. But now am I prepared to live?
Recovery from the surgery itself was easy. The psychic recovery less so. Several weeks ago, I found myself crying unreasonably about a bruised rib, unrelated to but near my healed sternum. Taken by surprise at an emotional response greater than the bruise deserved, I insisted to my husband that it was connected to the bypass. Yet I knew full well that it was not. Patients and families must not rush past the pain that is part of living—for Christians, it can be how we enter into the suffering of Jesus.
The dignity of the patient must be respected and honored. Between the assault on the patient’s body and the insults to her intelligence, she can be reduced to a thing, a nonresponsible biological entity. The heart in Room 3. Of course, vulnerability accompanies any medical situation. But, when one is perceived—sometimes rightly—as less informed, it is difficult to formulate intelligent questions, much less summon the decision-making power, to take control of one’s own medical destiny. Our health-care system must do more than remind patients of follow-up appointments and eagerly offer new medicines and treatments. Medical professionals must understand that patients continue to feel profound distress from the trauma their bodies experienced. Such wounds go deeper than scalpel cuts. And like the fading scars on my body, their healing may never be complete.
