It’s been a little more than six years since Republican senator John McCain of Arizona cast the dramatic “thumbs-down” vote that doomed his party’s attempt to repeal the Affordable Care Act and preserved health care for millions of Americans. Obamacare may be imperfect, with its patchwork of providers and marketplaces and confusing plan tiers. But it is beyond question that it has done a lot of good, insuring some twenty million Americans, expanding access to Medicaid for poor and working-class people, and offering much-needed protections to women, young people, seniors, rural communities, and those with preexisting conditions. It’s become so popular, even among many conservative voters, that Republican politicians don’t dare talk of repealing it anymore.
Less dramatic than McCain’s vote, but no less meaningful, was the Biden administration’s announcement in August that the federal government under Medicare would soon begin negotiating the prices of ten prescription drugs, including treatments for diabetes, heart disease, and blood cancer. First passed as part of the 2022 Inflation Reduction Act, the provision is an important step toward achieving fairer health-care outcomes in the United States, where prescription drugs cost an average of 2.56 times more than in other countries, and where medical expenses cause the overwhelming majority of personal bankruptcies. Patients needing these ten drugs (and the twenty or so other medications to be added each year) won’t be the only beneficiaries; beginning in 2025, those requiring insulin will see their out-of-pocket expenses capped at $35 per month, while yearly costs for drugs taken at home will be limited to $2,000 for all Medicare recipients. The savings accruing to taxpayers—the federal government estimates $160 billion over ten years—could be reinvested in the American health-care system, lowering costs for everyone.
This overdue measure has sparked predictable outcry from pharmaceutical companies. Sensing a threat to their outsized profit margins, among the highest of all industries, they’ve filed lawsuits, engaged in fear mongering, and pushed outright lies. Some of their arguments—that having to negotiate a fair price with Medicare violates their right to free speech, or that they’re being subject to price controls and threatened with seizure of property—can be dismissed out of hand. Losing the right to dictate terms hardly constitutes coercion or theft. If anyone has been ripped off, it’s the federal government and the taxpayers who fund it. Since 2003, when Bush-era legislation expressly prohibited the federal government from using its considerable leverage to secure better prices, Medicare has been forced into the role of a “price taker.” The new provisions simply level the playing field, permitting the United States to do what it already does with other federal agencies and areas of medicine. If Medicare and the Departments of Defense and Veterans Affairs already negotiate prices for doctor visits, surgeries, and hospital stays, why should pharmaceuticals remain exempt? Besides, if drug companies really prefer not to do business with the government, they don’t have to—though they would be forgoing their largest source of revenue.
More pernicious are Big Pharma’s claims that if the courts don’t block negotiated prices, the cost of private insurance will jump and drug companies’ investment in research and development for lifesaving treatments will plunge. Neither claim stands up to scrutiny. Economists point out that if pharmaceutical companies could raise prices, they’d have done so already. In fact, the prices most private insurers pay for prescription drugs will probably go down, since insurers usually base what they pay on what Medicare pays. And it’s not as if Big Pharma leads the way in R&D spending or in patents. Giants like Pfizer, Merck, Johnson & Johnson, GSK, and BMS spend far more on sales, marketing, and lobbying than they do on R&D. It’s the federally funded National Institutes of Health that leads the world in funding medical research, especially at pivotal earlier stages. Imagine how much more it could do with the billions gained from savings on prescription drugs.
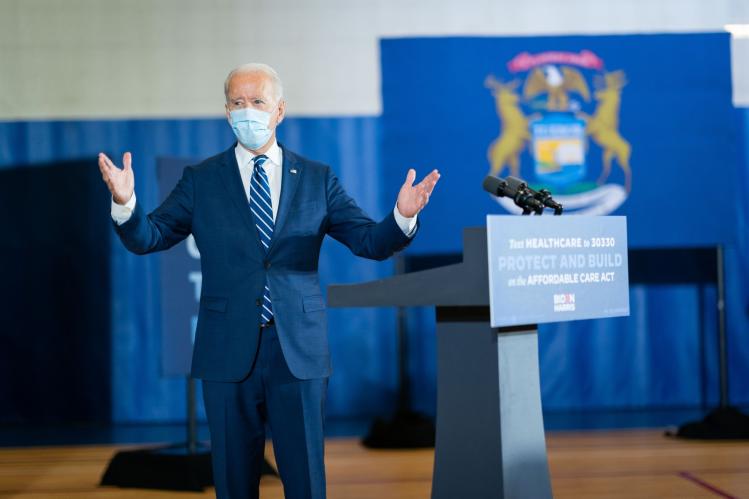
Polling shows that about 80 percent of Americans approve of the prescription-pricing plan, and President Biden has signaled that he’ll make drug pricing a centerpiece of his 2024 campaign. He should continue to press the issue of health care, which is a winning one for Democrats and which Republicans are largely silent on. Significant problems remain: too many Americans lack access to affordable mental-health care; administrative overhead and waste accounts for nearly 30 percent of the nation’s total annual medical expenditures; fraud makes up 10 percent of what the government spends on health care. Then there’s the chronic understaffing in hospitals and clinics, the for-profit takeover of the hospice industry, and the rise of private-equity funds buying up everything from nursing homes to fertility clinics, to the detriment of patients and providers alike. But reining in the pharmaceutical industry is an important step toward making health care more affordable for everyone. It’s also an indication that there’s the political will for the government to stop padding corporate profits.
